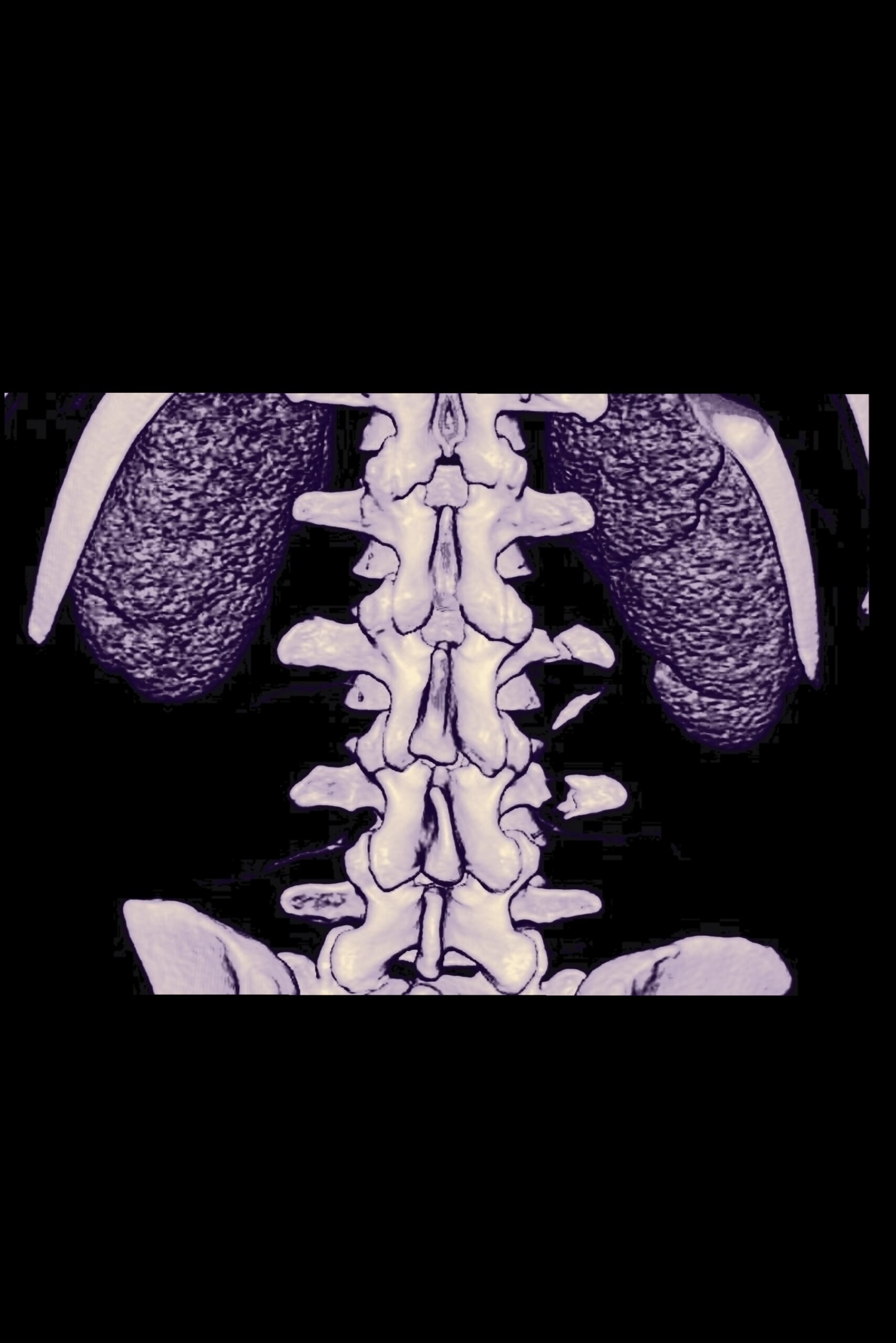
Magnetic resonance imaging (MRI) is a radiation-free, noninvasive imaging technique that provides threedimensional (3D) visualization of tissues. Its superior soft tissue contrast has made it a preferential diagnostic tool for the imaging of various organ systems, including the musculoskeletal system. On the other hand, osseous structures are usually visualized using radiography or computed tomography (CT). For imaging complex structures, CT is preferred as it offers high-resolution 3D images with a radiodensity contrast that highlights bony tissues.

CT images, in particular 3D bone renderings, have proven valuable in the diagnosis and treatment of bone pathologies, but pathologies affecting both soft and hard tissues, including skull, spine and joint disorders often warrant the acquisition of both MR and CT images. Recent advances [1] in MR image acquisition and processing, facilitated by the development of new hardware and the increase in computing power, have improved the bone contrast on MR images, making MRI a radiation-free alternative to CT for the diagnosis and treatment planning of certain musculoskeletal pathologies.
Going through apllications [1], CT is considered the modality of choice for visualizing cortical bone in 3D. However, its adverse radiation burden has motivated the research into alternative modalities with lower radiation doses, including radiography-based, low-dose CT-based, or MR-based methods. In this competition, despite some challenges in the acquisition, MRI has favorable properties including its superior soft tissue contrast that can be exploited to concurrently assess the soft tissue involvement of musculoskeletal pathologies without the need for image registration, and the complete absence of ionizing radiation.
It can be said that the utility of MRI as an imaging modality for visualizing bone has been shown in many areas of the human body. MRI presented several advantages compared to CT in the diagnosis of musculoskeletal pathologies. For example, immature bone as seen in the femur and pelvis of young children was better visualized on MR than on CT images. Than, MRI can acquire soft tissue and bone information in a single examination. Finally MR sequences for imaging bone can also be combined with other sequences for specific imaging such as venous or fluid-sensitive imaging, magnetic resonance angiography, or quantitative susceptibility mapping for a more comprehensive diagnosis within a single modality.

The use of an MR-based bone visualization could in the future be extended to facilitate clinical care motivated by the benefits of CT/MR fusion. Such fusions could be useful for the design of patient-specific implants by combining bone and joint capsule information and have proven their potential for diagnostic and treatment purposes, by easing the diagnosis for junior readers, and by facilitating treatment guidance and surgical navigation [1].
MRI will probably not replace CT for all its applications in the near future, in emergency settings CT is still the most popular technique. However, for clinical indications where both bone and soft tissue information are required, these new approaches open new perspectives.
[1] Magnetic Resonance Imaging Versus Computed Tomography for Three-Dimensional Bone Imaging of Musculoskeletal Pathologies: A Review. – Mateusz C. Florkow, MSc, Koen Willemsen, MD, Vasco V. Mascarenhas, MD, PhD, Edwin H.G. Oei, MD, PhD, Marijn van Stralen, PhD and Peter R. Seevinck, PhD; J. MAGN. RESON. IMAGING (2022);56:11–34.